Geographical distance, limited health human resources, and complex health and social issues are some of the challenges faced by health practitioners in rural and remote regions of British Columbia (BC). Having worked for over 15 years as a physiotherapist (PT) in rural BC, former trainee Robin Roots has first-hand experience of what it means to tackle them in practice and through research.
Here, she updates us on the latest goings-on in her research:
 What led you to focus your research on rehabilitation practices and services in rural BC?
What led you to focus your research on rehabilitation practices and services in rural BC?
Working as a PT on Northern Vancouver Island and in the communities of Kitimat and Prince Rupert, I encountered challenges to providing services with limited resources and support. As a physio, I’ve always felt I have an enormous role to play in addressing issues around health inequity, access to services and health literacy.
Plus, I recognized that I might be able to improve access to and availability of care through research in rehabilitation practice and service.
How is your research working to address key issues?
Under the supervision of Dr. Linda Li, I conducted a qualitative study designed to construct an understanding of rural rehabilitation practice from the perspective of occupational therapists (OTs) and PTs working in rural and remote BC. This greater understanding can now inform an educational framework for rural practice.
Also, partnerships with the University of Northern British Columbia and Northern Health are enabling the expansion of physiotherapy training to northern and rural B.C. These developments present exciting opportunities to influence practice education for physiotherapy students and to support the continuing education of practising physiotherapists. Ultimately, these partnerships offer the chance to improve health services in rural communities through recruitment, retention and linking education to practice.
I am now charged with designing, implementing and evaluating the University of Northern British Columbia’s Northern and Rural Cohort, as part of a new initiative to provide students with clinical education opportunities in northern and rural BC. My research informs my teaching role, in which I introduce students to rural health issues, determinants of health, cultural safety and competencies for rural practice.
Can you summarize the main findings of your research so far?
From interviews with OTs and PTs, I learned that rural practitioners overcome resource shortages by practising to the full 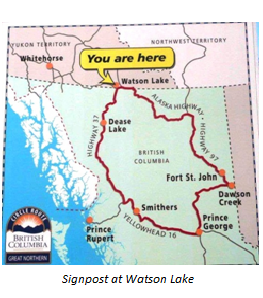 extent of their scope, frequently ‘stretching their roles’ to cover gaps in care, and collaborating with other health providers to meet the needs of the rural population. The practice of OTs and PTs who participated in my research resembles primary health care in its approach to community and population health.
extent of their scope, frequently ‘stretching their roles’ to cover gaps in care, and collaborating with other health providers to meet the needs of the rural population. The practice of OTs and PTs who participated in my research resembles primary health care in its approach to community and population health.
My research also provided insight into how the rural context shapes, influences and challenges rural practice. My interviews with therapists identified continuing professional development as a major challenge that is not necessarily overcome by the greater use of technology. Hands-on education and in-person mentoring programs are also needed.
What are the next steps for your research?
In my current role as Coordinator of Clinical Education for the UBC Masters of Physical Therapy Northern and Rural Cohort, I’m able to draw on my research and contribute to the development of a curriculum that focuses on rural health issues. Building innovative programming to expand placement capacity in rural communities is also allowing me to explore aspects of my research further, such as the role of PTs in primary health care in rural communities.
I also continue to be involved in a number of research projects. One example is the Interprofessional Rural Program of BC, which assesses interprofessional education for collaborative practice in rural communities.